The meticulous compounding of hazardous medicines is a critical aspect of healthcare, demanding the highest quality standards to ensure patient safety and treatment efficacy. This article aims to present how these standards are upheld within the British healthcare system.
The Regulatory Framework for Compounding Hazardous Medicines in the UK
In the UK, a carefully structured regulatory framework governs the compounding and administration of hazardous medicines. Here’s a detailed breakdown of the key organizations involved and how they interact with each other.
Medicines and Healthcare Products Regulatory Agency (MHRA)
Primary Role: The MHRA stands at the forefront, overseeing all aspects of medicine and medical device regulations across the UK.
Interactions: It sets the overarching standards and guidelines, directly influencing the operations and practices of other regulatory bodies like the GPhC, PASG, and BOPA.
The main responsibilities of the MHRA for compounding hazardous medicines include:
- Setting Standards and Guidelines: Developing and enforcing guidelines for the safe compounding of hazardous drugs, ensuring adherence to Good Manufacturing Practice (GMP) standards.
- Quality Assurance: Overseeing the quality management systems in pharmacies and hospital settings to ensure that compounded medicines meet the required safety and quality standards.
- Monitoring and Inspection: Conducting regular inspections of compounding facilities to ensure compliance with regulatory requirements and GMP.
- Pharmacovigilance: Implementing robust pharmacovigilance systems to monitor adverse drug reactions and ensure timely reporting and action on any safety concerns associated with compounded medicines.
- Enforcement and Compliance: Taking appropriate enforcement actions against non-compliance and ensuring that pharmacies and hospitals adhere to the established compounding standards and regulations.
General Pharmaceutical Council (GPhC)
Primary Role: This council regulates pharmacy professionals and pharmacies, ensuring compounding processes meet the highest safety and quality standards.
Interactions: Working in line with MHRA’s regulations, the GPhC is responsible for implementing these standards at the pharmacy level, collaborating closely with the PASG to ensure compliance and enforcement.
The main responsibilities of the GPhC in regulating the compounding of hazardous medicines include:
- Setting and Enforcing Standards: Establishing clear, rigorous standards for the compounding of hazardous drugs in pharmacies and hospitals.
- Inspection and Monitoring: Regularly inspecting pharmacy facilities to ensure compliance with compounding standards and safe practices.
- Guidance and Training: Providing guidance and resources for pharmacy professionals regarding the safe compounding of hazardous drugs, including training requirements.
- Quality Assurance: Ensuring that pharmacies have robust quality assurance processes in place for the compounding of hazardous drugs.
- Pharmacy Registration and Compliance: Overseeing the registration of pharmacies and ensuring they comply with the legal and professional requirements for compounding hazardous drugs.
- Risk Management: Implementing and enforcing risk management strategies to minimise the risks associated with the compounding of hazardous drugs.
British Pharmacopoeia Commission (BPC)
Primary Role: The BPC sets the quality standards for medicinal substances, fundamental for compounding processes.
Interactions: It provides the scientific basis for MHRA’s regulations, guiding the Expert Advisory Groups in advising on best practices for medicinal products.
Key responsibilities of the British Pharmacopoeia Commission (BPC) include:
- Standard Setting for Medicinal Substances: Developing and maintaining the British Pharmacopoeia, which provides the official standards for the quality of medicinal substances, including those used in compounding hazardous drugs.
- Guidance on Formulations: Offering detailed guidance on the formulation of medicines, ensuring that compounded drugs meet the necessary quality and safety standards.
- Ensuring Consistency and Quality: Ensuring the consistency and quality of medicinal substances and preparations, which is critical in the compounding process, especially for hazardous drugs.
- Updating Standards: Regularly updating and revising the standards in the British Pharmacopoeia to reflect advancements in pharmaceutical science and technology.
- International Collaboration: Collaborating with international bodies to align the UK’s pharmaceutical standards with global best practices
BPC works in conjunction with the MHRA to align the standards with broader public health protections and medicine regulations.
For the latest information on the standards and guidelines set by the BPC, healthcare professionals and institutions like yours can refer to the British Pharmacopoeia, which is now legally effective. Check the 2024 edition here.
The Commission on Human Medicines
Primary Role: The Commission on Human Medicines is pivotal as an advisory body, providing critical guidance and recommendations to ensure the safe and effective use of medicinal products in the UK.
Interactions: It plays a significant role in advising the Licensing Authority, impacting the regulation of medicines by the MHRA. The Commission’s evaluations and recommendations directly inform the regulatory landscape for compounding hazardous drugs, influencing policy and practice at all levels.
Key responsibilities of the Commission on Human Medicines in this context include:
- Advisory Role: Providing expert advice to the Licensing Authority on the safety, quality, and efficacy of medicinal products, including those used in compounding hazardous drugs.
- Evaluation of Safety and Efficacy: Assessing the safety and efficacy of medicinal products, particularly those classified as hazardous, to ensure they meet the required standards for patient use.
- Risk-Benefit Analysis: Conducting risk-benefit analyses of medicinal products to guide decision-making processes regarding their use and compounding.
- Guidance on Medicinal Standards: Offering guidance on standards and best practices for the compounding and use of hazardous drugs, based on the latest scientific and clinical evidence.
- Monitoring Adverse Drug Reactions: Monitoring adverse drug reactions and other safety concerns related to compounded hazardous drugs and advising on appropriate actions to mitigate risks.
- Policy Recommendations: Making policy recommendations to regulatory bodies to enhance the regulatory framework governing the compounding of hazardous drugs.
Expert Advisory Groups (EAG)
Primary Role: These groups offer specialized advice on various aspects of medicinal products.
Interactions: They play an advisory role to both the MHRA and BPC, impacting the development and refinement of guidelines for hazardous drug compounding.
Appointed by the Commission on Human Medicines and the British Pharmacopoeia Commission the Expert Advisory Groups play a crucial consultative role in the regulation of compounding hazardous drugs in hospitals and pharmacies in the UK. They consist of experts in various fields of medicine and pharmaceuticals.
The main responsibilities of these Expert Advisory Groups include:
- Providing Specialized Advice: Offering expert guidance on specific issues related to the compounding of hazardous drugs, including safety, quality, and efficacy.
- Recommendations on Standards and Practices: Recommending standards and best practices for the compounding of hazardous drugs, ensuring they align with current scientific understanding and clinical evidence.
- Reviewing and Updating Guidelines: Assisting in the review and updating of guidelines and standards, particularly those published in the British Pharmacopoeia and other regulatory documents.
- Risk Assessment and Management: Contributing to the assessment and management of risks associated with the handling and compounding of hazardous drugs.
- Innovation and Research Support: Providing insights into the latest research and technological advancements that can impact the compounding of hazardous drugs and suggesting ways to incorporate these into current practices.
- Liaison and Coordination: Facilitating communication and coordination between the Commission on Human Medicines, the British Pharmacopoeia Commission, and other regulatory bodies to ensure cohesive and comprehensive regulation
The Licensing Authority
- Primary Role: The Licensing Authority, comprising the Secretary of State and the Minister for Health, Social Services, and Public Safety, is entrusted with the critical task of ensuring that the compounding of hazardous drugs in the UK adheres to stringent safety and quality standards.
- Interactions: It is the body responsible for the issuance and regulation of licenses for the manufacturing, assembling, or importing of medicinal products. By ensuring compliance, enforcing regulations, and updating policies, the Licensing Authority shapes the environment within which pharmacies and manufacturers operate, thus safeguarding public health.
Key responsibilities of the Licensing Authority include:
- Granting and Regulating Licenses: Issuing licenses for the manufacturing, assembling, or importing of medicinal products, including hazardous drugs.
- Quality and Compliance Oversight: Ensuring that licensed entities adhere to the required quality standards for compounding hazardous drugs.
- Regulation Enforcement: Enforcing regulations related to the compounding of hazardous drugs, including imposing penalties for non-compliance.
- Policy Formulation: Developing and updating policies and guidelines to ensure the safe handling and compounding of hazardous drugs.
- Monitoring and Auditing: Conducting inspections and audits of facilities to ensure compliance with established standards and regulations.
- Risk Management: Implementing risk management strategies to minimise potential hazards associated with the handling and compounding of hazardous drugs.
Pharmaceutical Aseptic Services Group (PASG)
Primary Role: The PASG focuses on aseptic preparation, upholding stringent standards for the compounding of hazardous drugs.
Interactions: It aligns its practices with the guidelines set by MHRA and GPhC, conducting audits and overseeing quality control in pharmacy environments.
This group operates under the framework of the Royal Pharmaceutical Society, focusing on establishing and maintaining high standards for aseptic preparation and ensuring the safety and efficacy of compounded drugs.
Key responsibilities of the Pharmaceutical Aseptic Services Group in regulating the compounding of hazardous medicines include:
- Standard Setting: Developing and maintaining standards for aseptic compounding of hazardous drugs, ensuring practices meet national and international guidelines.
- Quality Assurance and Control: Implementing quality assurance and control measures to guarantee the sterility and safety of compounded drugs.
- Risk Management: Establishing robust risk management protocols to minimise the risks associated with handling and compounding hazardous drugs.
- Training and Education: Providing specialized training and educational resources to healthcare professionals involved in aseptic compounding.
- Policy Development: Formulating policies and guidelines for the safe compounding of hazardous drugs, including the use of Personal Protective Equipment (PPE) and containment strategies.
- Monitoring and Compliance: Conducting regular audits and inspections to ensure compliance with established standards and procedures in aseptic compounding.
Royal Pharmaceutical Society (RPS)
Primary Role: The RPS establishes national standards for aseptic preparation services in the UK, ensuring the quality and safety of compounded hazardous medicines.
Interactions: Collaborates with the NHS Pharmaceutical Quality Assurance Committee to audit and assure the quality of pharmacy aseptic units, aligning with MHRA guidelines and supporting the framework established by the GPhC and PASG.
The RPS is instrumental in developing and maintaining national standards for the aseptic preparation of medicines, with a particular focus on ensuring the quality and safety of hazardous drug preparations. In close partnership with the NHS Pharmaceutical Quality Assurance Committee, the RPS has instituted quality standards and auditing processes to uphold the integrity of pharmacy aseptic units. While these standards are tailored to the NHS, they also provide a benchmark for educational purposes and international healthcare entities.
The main responsibilities of the RPS in regulating the compounding of hazardous drugs include:
- Developing national standards that guide aseptic preparation services.
- Overseeing the preparation of critical medicines, particularly in settings that involve unlicensed hospital aseptic preparation units.
- Collaborating to establish audit programs that maintain the high quality of aseptic units within the NHS.
- Advising on the practical application of these standards through resources such as the “Quality Assurance of Aseptic Preparation Services: Standards Handbook.”
British Oncology Pharmacy Association (BOPA)
Primary Role: BOPA specifically addresses oncology pharmacy practices, emphasizing the safe compounding and administration of hazardous drugs in this field.
Interactions: Operating under MHRA’s regulatory framework, BOPA collaborates with both the NHS and UKONS to develop specialized training and policies for oncology-related scenarios.
BOPA plays a significant role in guiding and influencing the practice of compounding hazardous drugs, particularly in the field of oncology, within hospitals and pharmacies in the UK. BOPA’s focus is on enhancing patient care and safety in cancer treatments, where handling and compounding hazardous drugs, like chemotherapy agents, require stringent protocols.
The main responsibilities of BOPA in this context include:
- Setting Clinical Standards: Developing and advocating for clinical practice standards in oncology pharmacy, particularly regarding the safe compounding and administration of hazardous drugs.
- Providing Education and Training: Offering educational resources and training programs to oncology pharmacy professionals for safe and effective compounding practices.
- Promoting Research and Best Practices: Encouraging research in oncology pharmacy and disseminating best practice guidelines for compounding hazardous drugs.
- Quality Assurance and Safety: Focusing on quality assurance measures to ensure the safety and efficacy of compounded oncology medications.
- Policy and Guidance Development: Contributing to the development of policies and guidance related to oncology pharmacy, including the handling and compounding of hazardous drugs.
- Collaboration with Regulatory Bodies: Working alongside healthcare regulatory bodies to influence policy decisions and regulations governing the compounding of hazardous drugs in oncology.
National Health Service (NHS)
Primary Role: The NHS oversees broader healthcare practices in the UK, including the safe compounding of hazardous drugs within NHS facilities.
Interactions: It implements safety protocols and training by MHRA guidelines and coordinates with entities like UHB to enforce local policies and procedures.
NHS in the UK plays a critical role in regulating the compounding of hazardous drugs in hospitals and pharmacies. This involves overseeing practices to ensure the safety and efficacy of drug preparation, particularly when dealing with cytotoxic and other chemotherapeutic agents that pose significant risks to both healthcare providers and patients.
The main responsibilities of the NHS in this context include:
- Establishing Safety Protocols: Implementing comprehensive safety protocols for the handling, compounding, and administration of hazardous drugs.
- Staff Training and Education: Providing extensive training and education to healthcare staff, emphasizing the safe handling of hazardous drugs and the use of Personal Protective Equipment (PPE).
- Quality Assurance: Ensuring quality assurance in the compounding process, including adherence to aseptic techniques and proper storage conditions.
- Risk Assessment and Management: Conducting risk assessments to identify potential hazards and implementing strategies to mitigate these risks.
- Regulatory Compliance: Enforcing compliance with relevant laws and regulations, including COSHH (Control of Substances Hazardous to Health) regulations, and ensuring adherence to NHS policies and guidelines.
- Monitoring and Auditing: Regularly monitoring and auditing pharmacy aseptic services and compounding units to ensure compliance with safety standards.
United Kingdom Oncology Nursing Society (UKONS)
Primary Role: UKONS concentrates on standardizing practices among oncology nurses, particularly in administering Systemic Anti-Cancer Therapy (SACT).
Interactions: It ensures that nursing practices align with the standards set by BOPA and the training requirements of the NHS, enhancing the safe administration of oncology treatments.
UKONS plays a pivotal role in regulating the process of compounding hazardous drugs, particularly Systemic Anti-Cancer Therapy (SACT), in hospitals and pharmacies across the UK. The SACT Competency Passport, developed by UKONS, serves as a key tool in this regulation.
The main responsibilities of UKONS in the context of compounding hazardous drugs include:
- Standardizing Competencies: Developing and updating the SACT Competency Passport to ensure a standardized level of knowledge and skill among healthcare professionals handling and administering SACT.
- Promoting Safe Handling of SACT: Emphasizing the safe handling and administration of SACT to minimize occupational exposure risks to healthcare professionals.
- Education and Training: Providing theoretical and practical guidance for the education and training of nurses and other healthcare professionals in the safe administration of SACT.
- Clinical Practice Assessment: Implementing a structured approach for clinical practice assessment to ensure practical proficiency in SACT administration.
- Annual Reaccreditation: Instituting a process of annual reaccreditation to maintain and update competencies in SACT administration.
- Patient-Centred Care Focus: Highlighting the importance of patient-centred care during SACT administration, including patient education and support.
- Adaptability to Various Settings: Ensuring that the competencies and guidelines are adaptable to different healthcare settings and roles involved in SACT administration.
- Feedback and Continuous Improvement: Encouraging feedback and ongoing improvement of the SACT Competency Passport to align with evolving practices and patient needs in oncology care.
University Hospitals, Pharmacies and Compounding Centres
Primary Role: They represent the practical application of these standards in a healthcare facility setting, focusing on safety procedures and staff training.
Interactions: It adopts and implements policies and procedures in line with NHS and MHRA guidelines, ensuring local compliance and effective risk management.
University Hospitals, pharmacies and compounding centres focus predominantly on establishing rigorous protocols and procedures to manage the risks associated with handling and administering cytotoxic and chemotherapeutic agents.
Their main responsibilities in this context include:
- Developing Safe Handling Procedures: Establishing detailed procedures for the safe prescribing, handling, and administration of cytotoxic and other chemotherapeutic agents.
- Staff Training and Competency: Ensuring that medical, nursing, and pharmacy staff are adequately trained and deemed competent in handling hazardous drugs, including specific training for chemotherapeutic agents.
- Patient Safety and Consent: Implementing procedures to ensure patient safety, including informed consent processes for patients undergoing treatment with hazardous drugs.
- Risk Assessment and Management: Performing thorough risk assessments and management strategies for the use of hazardous drugs in various clinical settings.
- Quality Control and Assurance: Overseeing the quality control processes for compounding hazardous drugs, ensuring compliance with aseptic techniques, and correct storage and handling.
- Policy Development and Compliance: Developing and maintaining policies in line with national guidelines and regulatory requirements for the safe handling of cytotoxic drugs.
- Monitoring and Reporting: Regularly monitoring the handling and administration of hazardous drugs and ensuring the reporting and management of any related incidents or near misses.
This integrated network, led by the MHRA, and supported by organizations like the GPhC, PASG, BOPA, NHS, and all the others mentioned above ensures that the compounding and administration of hazardous drugs in the UK are not only safe and effective but also centred around the needs of patients.
How to Apply Good Manufacturing Practice (GMP) Standards When Compounding Hazardous Medicines
Understanding Good Manufacturing Practice in Compounding Hazardous Medicines
In the intricate world of pharmaceutical compounding, Good Manufacturing Practice (GMP) stands as a beacon of quality and safety. Particularly in the compounding of hazardous medicines, GMP is not just a set of guidelines but a vital framework ensuring that every medication is produced with the highest standards of safety and efficacy. This introduction sets the stage for understanding how GMP standards are meticulously applied in the compounding of hazardous drugs.
The Role of GMP in Ensuring Consistency, Quality, and Safety for Healthcare Workers Compounding Hazardous Drugs
By following the GMP standards, pharmacies and healthcare facilities can:
- Minimize contamination risks.
- Ensure accurate dosing and ingredient mixing.
- Maintain an environment that protects both the product and the healthcare professionals involved in compounding.
- Uphold stringent quality control throughout the compounding process.
Specific GMP Requirements for UK Compounding Pharmacies and Outsourced Facilities
Compounding pharmacies in the UK, along with outsourced facilities dealing with hazardous drugs, must adhere to specific GMP requirements. Key steps include:
- Comprehensive Risk Assessment: Identify potential hazards in compounding processes and implement appropriate safety measures.
- Qualified Personnel: Ensure that staff are adequately trained in handling hazardous materials and understand GMP principles.
- Facility Design and Maintenance: Design facilities to prevent cross-contamination. Regular maintenance and cleanliness are paramount.
- Equipment Validation: Validate all equipment used in compounding to ensure accuracy and safety.
- Detailed Documentation: Maintain thorough records of compounding processes, ingredient sourcing, and staff training.
- Regular Auditing and Inspection: Periodic audits and inspections are essential to ensure ongoing compliance with GMP standards.
- Quality Control Measures: Implement rigorous testing procedures for both raw materials and finished products.
- Reporting and Addressing Non-Compliance: Establish protocols for reporting GMP violations and taking corrective actions.
For a more comprehensive understanding of GMP and its application in compounding hazardous medicines, further resources and training are recommended.
Best Practices in Quality Control and Assurance for Compounding Hazardous Drugs
Next, we shift our focus to the twin pillars of quality control (QC) and quality assurance (QA) in the compounding of hazardous drugs. This part of the article emphasizes the critical role these practices play in ensuring that compounded medications not only meet safety standards and comply with GMP but also retain their intended efficacy, especially in high-risk scenarios like aseptic preparations.

The Crucial Role of Quality Control and Assurance
Quality control and assurance in compounding hazardous medicines are paramount due to the high risks involved. As per NHS England’s guidelines, stringent QC and QA practices ensure that compounded medications meet the necessary safety, quality, and efficacy standards (NHS England). This is especially vital in aseptic preparations where the risk of contamination can have dire consequences.
Quality Control Procedures: A Closer Look
Testing
Regular and thorough testing is a cornerstone in compounding hazardous drugs. This includes sterility tests, endotoxin tests, and potency checks, as emphasized by the Specialist Pharmacy Service (SPS).
Documentation and Record-Keeping
Meticulous documentation is key. This encompasses compounding procedures, outcomes, and any deviations or incidents.
The NHS England guidance underlines the importance of digital platforms like iQAAPS for effective documentation and compliance management.
Equipment and Processes Validation
Equipment and processes require regular validation to ensure consistent quality. This includes clean rooms, sterilization processes, and compounding techniques.
Validation ensures that every aspect of the compounding process adheres to predefined standards and is capable of consistently delivering quality products.
Operator Training and Validation
Compounding personnel must be adequately trained and periodically revalidated to maintain proficiency in handling hazardous drugs.
As per NHS England’s guidance, this includes assessing and ensuring staff competence in aseptic techniques and handling hazardous substances (NHS England).
Adherence to Standards and Guidelines
Following established standards, such as those outlined in the “Quality Assurance of Aseptic Preparation Services” by the Royal Pharmaceutical Society and the NHS Pharmaceutical Quality Assurance Committee, is crucial (RPS).
These standards provide a comprehensive framework covering all aspects of aseptic preparation, including risk management, equipment validation, and staff training.
Risk Management and Compliance in Compounding Hazardous Medicines
Understanding the Risks in Pharmaceutical Compounding
The compounding of hazardous drugs in pharmaceutical manufacturing presents a unique set of challenges, demanding meticulous risk management and unwavering compliance with regulatory standards. These processes are critical for ensuring the safety and effectiveness of medications, while also safeguarding the health of those involved in their preparation.
The Critical Role of Risk Assessment
Risk assessment is the cornerstone of managing potential hazards in pharmaceutical manufacturing, particularly in the compounding of hazardous drugs. It involves a systematic evaluation of processes to identify potential risks to both product quality and personnel safety.
Identifying Hazards
This initial step involves recognizing all possible risks associated with the compounding of hazardous drugs, ranging from chemical toxicity to environmental contamination.
The identification of hazards in pharmaceutical compounding requires a multi-faceted approach:
Comprehensive Inventory: Begin by creating a comprehensive inventory of all substances used in the compounding process. This includes active pharmaceutical ingredients, excipients, and any cleaning agents. Reference the Control of Substances Hazardous to Health (COSHH) Inventory Document for guidance on documenting substances.
Material Safety Data Sheets (MSDS): Obtain and review the MSDS for each substance, which provides crucial information on chemical properties, toxicity, handling, storage, and disposal requirements.
Workplace Exposure Limits (WELs): Consult the latest WELs, which are legal limits on the amounts of hazardous substances in the air, as provided by the HSE guidelines, to assess airborne risks.
Process Analysis: Analyse the compounding process step by step to identify where and how workers might be exposed to hazardous substances. This includes examining handling procedures, the potential for aerosol generation, and points of environmental release.
Consultation with Experts: Engage with health and safety committees, pharmacists, and industrial hygienists to review procedures and identify potential hazards that may not be immediately obvious.
Equipment Review: Ensure that all equipment used in the compounding process is examined for containment efficacy. Closed-system drug-transfer devices (CSTDs) should be considered to minimize exposure.
Legislative Framework: Familiarize yourself with the legislative framework relevant to hazardous drug compounding, such as the COSHH regulations and any specific guidance for pharmaceuticals, to understand the legal requirements for hazard identification.
Cytotoxic Specificity: For cytotoxic drugs, refer to specialized guidance like the HSE’s “Safe handling of cytotoxic drugs in the workplace” to understand specific risks associated with these potent compounds.
Evaluating Risks
Once potential hazards are identified, the next critical phase is risk evaluation. This process quantifies the likelihood and severity of the identified risks and their potential impact on both product quality and personnel safety. Here’s how to approach this:
Use of Risk Matrices: Employ risk matrices to gauge the severity of the hazard and the likelihood of its occurrence. This method combines qualitative and quantitative assessments to prioritize risks.
Consult WELs and Occupational Exposure Limits: Refer to Workplace Exposure Limits and Occupational Exposure Limits for hazardous substances as outlined by HSE guidelines, to determine acceptable levels of exposure and assess the extent to which current practices exceed these benchmarks.
Quantitative Exposure Assessments: Perform quantitative exposure assessments for tasks that involve handling hazardous drugs. This includes air monitoring for volatile substances and surface contamination assessments for non-volatile compounds.
Health Surveillance Data: Review health surveillance data, if available, to understand the historical impact of substance exposure on employees’ health. This data can highlight trends and help assess the potential chronic health risks.
Severity of Consequences: Assess the severity of potential adverse events on both health and the environment. For instance, consider the implications of exposure to reproductive toxins or the impact of a chemical spill.
Exposure Duration and Frequency: Evaluate the duration and frequency of exposure to hazardous substances. This includes considering both routine operations and the potential for accidental exposures.
Mitigation Efficacy: Examine the current control measures in place for their effectiveness. Review incident reports and near-misses to evaluate if current mitigation strategies are sufficient.
Consultation with Regulatory Bodies: For complex risk evaluations, consider consulting with regulatory bodies or external experts. They can provide insights into risk assessment methodologies that are compliant with current regulations.
Task-Specific Risks: Use task-based risk assessments for activities involving hazardous drugs, as recommended by the Royal Pharmaceutical Society. This approach looks at the risks associated with the compounding process itself.
Documentation and Review: Document all findings thoroughly. This documentation should be readily accessible for review and use in future risk assessments and audits.
By taking these practical steps, organizations can systematically evaluate the risks associated with the compounding of hazardous medicines. This evaluation not only informs the implementation of appropriate safety measures but also ensures that risk mitigation strategies align with the latest health and safety standards, thereby safeguarding both product integrity and occupational health.
Implementing Mitigation Strategies
Based on the risk evaluation, appropriate mitigation strategies are developed. These may include engineering controls, like closed-system drug-transfer devices, administrative controls, and the use of personal protective equipment (PPE).
Continuous Monitoring and Review
Risk assessment is an ongoing process. Regular monitoring and review are crucial for ensuring the effectiveness of the mitigation strategies and for adapting to any changes in processes or regulations.
The Imperative of Regulatory Compliance
Compliance with regulatory guidelines is not just a legal obligation but a moral imperative in pharmaceutical manufacturing. The guidelines provided by agencies like the Health and Safety Executive (HSE) and the Royal Pharmaceutical Society are designed to prevent adverse events, ensuring the highest standards of safety and efficacy in drug compounding.
Sterile vs. Non-Sterile Compounding Practices
Sterile vs. Non-Sterile Compounds: Understanding the Basics
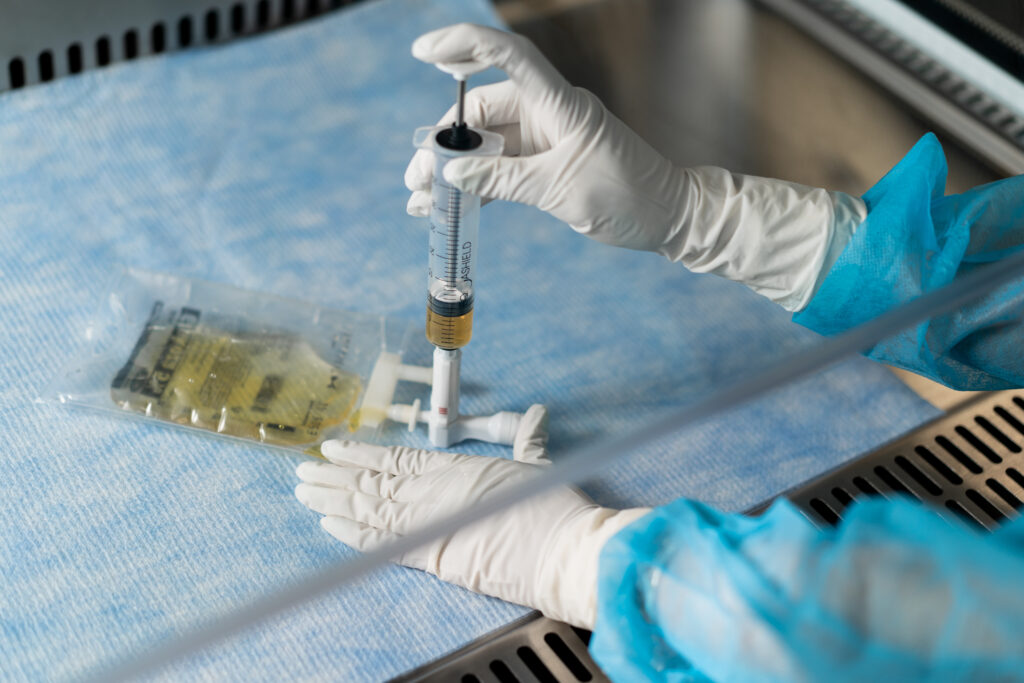
Sterile Compounds are medications prepared under strict aseptic conditions to ensure they are free from all forms of microbial life. These compounds are typically used in injections, eye preparations, and other routes of administration where sterility is paramount for patient safety.
Non-sterile compounds, in contrast, are prepared in a less stringent environment. They include oral medications, ointments, and creams where absolute sterility isn’t a necessity, though quality and safety remain crucial.
Regulations and Best Practices for Sterile Compounding
Aseptic Techniques and Cleanroom Standards
When it comes to sterile compounding, aseptic techniques are the cornerstone. As outlined in the “Guidance for ‘specials’ manufacturers” by the UK Government, these techniques involve meticulous practices to avoid contamination, including proper hand hygiene and the use of sterilized equipment (GOV.UK).
The environment where sterile compounding occurs is equally vital. Cleanrooms or controlled environments, adhering to standards such as ISO Class 5, are essential. These spaces are designed to maintain low levels of environmental pollutants and are equipped with High-Efficiency Particulate Air (HEPA) filters to ensure air purity, as emphasized in the “Transforming NHS Pharmacy Aseptic Services in England” report (NHS England).
Closed System Transfer Devices (CSTDs)
The use of CSTDs is a critical aspect of handling sterile products, particularly in oncology pharmacy. These devices prevent contamination during the transfer of medication from one container to another, ensuring the sterility of the product and safeguarding healthcare workers from exposure to hazardous drugs.
Sterility Testing
A fundamental component of quality control in sterile compounding is sterility testing. This process involves checking compounded sterile preparations for microbial contamination, ensuring the safety and efficacy of the medication for patient use. The rigorous standards for sterility testing are part of the broader regulatory framework outlined in “The Human Medicines Regulations 2012” (Legislation.gov.uk).
The distinction between sterile and non-sterile compounding is more than just a procedural difference; it’s about ensuring patient safety and medication efficacy. Adhering to stringent regulations and best practices, from aseptic techniques to cleanroom standards and sterility testing, is paramount in the pharmaceutical industry. By following these guidelines, pharmacists and technicians contribute significantly to delivering safe and effective personalized medication therapies.
Labelling and Packaging Requirements for Compounded Hazardous Medicines
Moving beyond the compounding process, we must consider the critical aspects of labelling and packaging of compounded hazardous medicines. This section will highlight the stringent regulations governing labelling and the importance of accurate and informative packaging in maintaining product integrity and ensuring patient safety.
Labelling Regulations for Compounded Pharmaceuticals
Compounded pharmaceuticals, particularly cytotoxic drugs used in cancer treatment and other diseases, require stringent labelling regulations. According to the “Human Medicines Regulations 2012“, all medicinal products, including compounded ones, must be clearly labelled. This labelling should include essential information such as the name of the medicine, strength, route of administration, posology, and warnings. The regulations ensure that healthcare professionals and patients can easily identify the medicine and understand its proper use, minimizing the risk of medication errors.
Importance of Accurate Labelling for Patient Safety
Accurate labelling of compounded hazardous drugs is vital for patient safety. As these drugs can have teratogenic, genotoxic, and carcinogenic properties, improper handling or administration due to mislabelling can lead to severe consequences. The guidelines from “Hospital Pharmacy Europe” highlight the need for well-labelled packaging to prevent occupational exposure and ensure safe administration to patients. Labels must be informative and clear, allowing healthcare workers to recognize and handle these drugs safely.
Packaging Considerations for Product Integrity and Stability
The packaging of compounded hazardous medicines is as crucial as labelling. The “Human Medicines Regulations 2012” stipulate that packaging must not only be secure but also maintain the integrity and stability of the product. Specialized packaging is recommended to prevent material breakage and contain spillage, especially during transport from manufacturers to hospitals. For instance, some manufacturers use moulded plastic containers for cytotoxic agents to confine any contamination in case of spillage. This approach minimizes the risk of exposure to pharmacy storekeepers and other healthcare workers.
Pharmacovigilance and Reporting Adverse Events for Compounding Hazardous Medicines
Introduction to Pharmacovigilance in Compounded Product Safety
As we near the conclusion, the focus shifts to pharmacovigilance – the watchful eye ensuring the safety of compounded medicines. This segment will discuss the importance of adverse event reporting and how it contributes to improving patient safety and refining compounding practices, thereby playing a pivotal role in the realm of hazardous drug compounding.
Pharmacovigilance involves the science and activities related to detecting, assessing, understanding, and preventing adverse effects or any other medicine-related problem. This vigilance is particularly vital in the area of compounding hazardous drugs, where the risks are inherently higher due to the nature of the substances involved. The goal of pharmacovigilance in this context is to minimize risks, maximize benefits, and promote the safe and effective use of compounded hazardous medicines.
Adverse Event Reporting Requirements and Timelines for Compounded Hazardous Drugs
The reporting of adverse events in the context of compounded hazardous drugs is a critical component of pharmacovigilance. It is mandatory to report adverse events electronically, except in exceptional circumstances. For all veterinary medicines, including compounded hazardous drugs, serious adverse events, human adverse reactions, and unintended transmission of infectious agents must be reported on an expedited basis. The Marketing Authorisation Holder (MAH) is responsible for validating all reported adverse events to ensure that the minimum information required is included in the report. These reports should be followed up to obtain additional information relevant to the case as necessary.
In the UK, for example, serious adverse events in animals and all human reactions occurring must be reported promptly, and no later than 15 calendar days from receipt to the appropriate regulatory body. This expedited reporting is essential for timely intervention and mitigation of risks associated with the use of compounded hazardous drugs.
Contribution of Reporting to Improvement and Patient Safety in Compounding Hazardous Drugs
The systematic reporting of adverse events in the compounding of hazardous drugs is not just a regulatory requirement but a cornerstone for improving patient safety and drug efficacy. Each reported event provides valuable data that can be analysed to understand better the risks associated with compounded hazardous drugs. This information is crucial for identifying trends, potential safety concerns, and areas for improvement in compounding practices.
Through diligent reporting and analysis, pharmacovigilance activities contribute significantly to enhancing the safety profile of compounded hazardous drugs. They help in refining compounding processes, improving drug formulations, and developing better guidelines for safe handling and administration. Ultimately, this leads to a higher standard of care and protection for both patients and healthcare professionals who handle these medications.
Emerging Trends in Pharmaceutical Compounding
In the final stretch of our journey, we explore the emerging trends and challenges in pharmaceutical compounding. This section will delve into the evolving legislative landscape, technological advancements, and the challenges of adapting to these changes. It will underscore the importance of staying updated with regulatory changes and embracing new technologies to enhance the safety and efficacy of compounding hazardous medicines.
Legislative Trends
The landscape of hazardous drug handling in healthcare settings is undergoing significant transformation, driven by evolving regulatory frameworks worldwide. A notable example is the recent updates to the Clinical Oncology Society of Australia’s position on the safe handling of monoclonal antibodies, reflecting a global shift towards more stringent safety protocols. These changes mirror the principles outlined in the USP General Chapter <800>, which was revised in December 2017 to enhance patient and healthcare worker safety. This chapter provides a comprehensive set of standards for the entire lifecycle of hazardous drugs, from their receipt to disposal, ensuring a holistic approach to safety.
Technological Trends
The compounding of hazardous drugs is undergoing a significant transformation, thanks to technological advancements. A key development in this area is the use of Closed-System Drug-Transfer Devices (CSTDs), which are instrumental in preventing the release of hazardous drug particles into the environment during their preparation and administration. This innovation enhances safety measures significantly. Complementing this, there’s a growing trend towards automated compounding processes. These automated systems drastically reduce the need for direct contact with hazardous drugs, thereby minimizing exposure risks for healthcare professionals in hospital environments.
Challenges in Adapting to Regulations and Technology
Keeping Pace with Regulatory Changes
Adapting to the dynamic regulatory environment remains a formidable challenge for healthcare facilities globally. The complexity and frequency of updates, as exemplified by regulations like USP <800> and the evolving guidelines in Australia, demand constant vigilance and adaptability. Ensuring compliance necessitates ongoing education and training for healthcare professionals involved in the compounding and handling of hazardous drugs. It’s imperative for healthcare institutions to invest in continuous learning and stay informed about global best practices to effectively navigate these regulatory waters.
Technological Adaptation
The integration of new technologies like CSTDs and automated compounding systems into healthcare practices presents certain challenges. One of the primary concerns is the financial aspect, as these advanced technologies typically incur higher costs. Moreover, adopting these new systems and equipment involves a learning curve. It requires healthcare workers to undergo comprehensive training and develop new skills to effectively use these technologies. This adaptation is crucial for ensuring both the safety of the healthcare environment and the efficacy of drug-compounding processes.
Environmental and Safety Concerns
The manufacturing and compounding processes for hazardous drugs raise environmental and safety concerns. The challenge lies in implementing sustainable practices that align with regulatory standards while ensuring the safety of healthcare workers and patients. This includes managing waste effectively and minimizing the environmental footprint of compounding practices.
The Importance of Staying Updated
In the face of these trends and challenges, it is imperative for healthcare facilities and professionals to stay informed about regulatory changes and industry best practices. Regular training, attending seminars, and engaging with professional bodies are essential steps in this direction. Staying updated not only ensures compliance with regulations but also enhances the overall safety and efficacy of compounding hazardous medicines.
In conclusion, the compounding of hazardous medicines is entering a new era marked by stringent regulations and innovative technologies. Navigating this landscape requires a proactive approach in adapting to regulatory changes and embracing technological advancements. By doing so, we can ensure the highest standards of safety and care in the pharmaceutical industry, ultimately benefiting both healthcare professionals and patients alike. As we move forward, it is crucial for all stakeholders to collaborate and share knowledge, ensuring that the compounding of hazardous medicines continues to evolve in a safe, efficient, and compliant manner.