Method
Four groups of vials containing growth media were accessed with 770 Equashield® syringes. Each vial was accessed 10, 7 and 5 times respectively during 7 days using the Equashield® CSTD and 4ml were drawn off each time.
Before each of the 770 accesses, the access membranes of Equashield® Vial Adaptors were inoculated with (>103 CFU) with gram positive or gram negative bacteria respectively and were left to settle during ½ an hour on the membrane. Initially the Vial Adaptors were spiked onto the media-filled vials two days earlier and incubated, resulting in a total of 9 days of testing, from first spiking to last access, and a total of 770 tested Equashield® Syringes and vial accesses.
The tested vials were incubated once again after the 9 days of testing and examined to demonstrate the ability of the Equashield® CSTD to prevent vial contamination during 7 days of use. To further increase the challenge and the extreme use conditions, approximately a third of the tested Equashield® devices were old expired products.
Results
All tested media-filled vials were negative for growth of any microorganisms.
Introduction
Equashield® is a Closed System Transfer Device (CSTD) for the preparation and administration of hazardous drugs and it is cleared under FDA’s product code ONB for “closed antineoplastic and hazardous drug reconstitution and transfer systems”. It complies with NIOSH’s definition: “A drug transfer device that mechanically prohibits the transfer of environmental contaminants into the system and the escape of hazardous drug or vapor concentrations outside the system” 2.
As a CSTD that is designated for working with hazardous drugs, the compliance of Equashield® with especially the second part of NIOSH’s definition2 has been extensively tested in clinical and scientific studies and proven to be compliant, namely: “mechanically prohibits the escape of hazardous drug or vapor concentrations outside the system”. In order to achieve full closure of the Equashield® CSTD and contamination free connections, unprecedented mechanisms and design features were incorporated into the CSTD, which in turn created a natural advantage for the CSTD over conventional systems and methods, whereby the risk of the transfer of microbial contaminants into the system is minimized. In another aspect, the United States Pharmacopeia (USP) Chapter 797 standards1 mandate that singleuse or non-preserved drugs must be discarded 6 hours after first vial access, if the vial is accessed and remains in ISO class 5 air conditions, otherwise it must be discarded after 1 hour. The purpose of this USP standard1 is to provide patient protection by limiting the impact potential of any microbial contamination of the drug. On the other hand, it creates significant waste of partially used viable drugs, which in turn, increase financial expenditure. This includes the high-cost drugs which are discarded in spite of the fact that the majority of them remain chemically stable for days and weeks.
Published economical surveys demonstrate the obvious saving potential of the wasted drugs (in $Millions) if CSTDs can be proven capable of prohibiting the transfer of microbial contaminants into the drug vial to maximize the utilization of the drug. Furthermore, such savings can also finance the cost of the CSTDs.
The Phaseal® CSTD (Becton & Dickinson) has demonstrated the potential to prevent microbial ingress in vials up to 7 days in the following studies: “Utility of the PhaSeal Closed System Drug Transfer Device”, Derek M. McMichael et al., Am J Pharm Benefits. 2011;3(1):9-163; and “Second Look at Utilization of a Closed-System Transfer Device (PhaSeal)”, E. Thomas Carey et al., Am J Pharm Benefits. 2011;3(6):311-3184.
Basically in these studies3,4, vials containing growth media were accessed 5 times during 7 days and each time a transfer of a small portion from the vial content took place using the Phasealsup® CSTD under ISO 5 air conditions. Membrane disinfections and other standard aseptic techniques were used as well. The vials, simulating the drugs, were incubated after the 7 days of testing and examined to demonstrate the ability to prevent vial contamination during 7 days of use.

Pseudomonas Aeruginosa
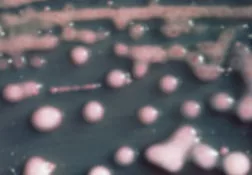
Klebsiella pneumoniae
Staphylococcus aureus

Aim
The aim of the current study was to perform a significantly more extreme-use-conditions test than worse conditions expected in hospital pharmacy settings and worse than conditions of the above referenced previous studies3,4 , thus assessing the ability of the Equashield® CSTD to prevent the contamination of parenteral drug products during 7 days of use.
Method
The challenge procedure consisted of inoculating the access membrane surface of multiple test article replicates of the Equashield® Vial Adaptor with gram positive or gram negative bacteria respectively, allowing the challenge to act and dry during ½ an hour, disinfecting the Vial Adaptor with a 70% isopropyl alcohol (IPA) pad, allowing the IPA to dry, connecting a new proprietary mating Equashield® 20ml Syringe Unit to the Vial Adaptor, and drawing a 4ml aliquot of sterile media (Soybean Casein Digest Broth) from the 50ml media-filled vial that the adapter was installed on. The test protocol specified a minimum inoculation titer of 103 colony forming units (CFU) per adaptor inoculation. The vials were divided into three similar groups and tested while the fourth group was added and tested in a replicated test one year later according FDA’s request. The first vial access was on day 1 at the commencement of the 9 day test, when the Vial Adaptors were spiked onto the sterile media-filled vials and then incubated two days long. Following their incubation and starting on day 3 the Vial Adaptors were each subjected to a total of 10 or 7 or 5 (group respectively) inoculation-disinfection-accesstransfer cycles over 7 calendar days, more specifically on days 3,4,5,8 and 9. The adapters were accessed once or twice each day, resulting in a total of 770 tested Equashield® Syringe Units with accesses and transfers.
The first three groups were tested with Staphylococcus aureus (American type Culture Collection ATCC #6538) and group four was tested in addition to S. aureus with Staphylococcus epidermidis, Klebsiella pneumoniae, Pseudomonas Aeruginosa.
To maintain equivalence with clinical use in hospital pharmacy, ISO 5 air conditions were used in this study and only one person for each group performed the testing without assistance. Furthermore, approximately a third of the tested Equashield® syringes and adapters were old products with expired use-dates. The tested vials were incubated for 2 days at 30°-35°C after the 9 days of testing and examined to demonstrate the ability of the Equashield® CSTD to prevent vial contamination during 7 days of use.
Results
All tested media-filled vials were negative for growth of any microorganisms.
Discussion
The results of the study confirmed that despite the extreme-use clinical conditions, the Equashield® CSTD prevented the microbial contamination of media-filled vials, which are more sensitive to contamination than drugs. The penetration of even one microorganism is suficient to create full contamination, and although the chances of bacteria survival and growth inside a hazardous drug vial are very slim, the media-filled vials used in the current study provided ample conditions for their multiplication and spreading.
To create even more extreme conditions, the vials in the current study were accessed up to 10 and 7 times during 7 days, whereas vials in previous studies3,4 were accessed only 5 times. Since the ability of a single connector to prevent contamination is naturally decreased with every additional connection and access, the number of connections gains increased significance in view of this non-linearly growing potential of contamination.
The repeated inoculation of the membrane with vivid bacteria before each of the vial accesses poses an extreme challenge to this primary microbial barrier; a challenge that does not exist (to such an extent) in a hospital routine setting, and that was also not included in the referenced studies3,4.
Without the special mechanisms and design features incorporated into the Equashield® connectors, the membrane alone would not be capable of such barrier performance. In fact, the doublemembrane connectors with their coring-free needles, special materials, and sequential guiding mechanisms, are responsible for creating the optimal conditions for satisfactory contamination prevention.
During the half hour that the bacteria were left to grow and settle on the membrane, the risk of them entering and settling in the openings or surface irregularities in the membrane, and subsequently moving into the vial or being moved by the penetrating needle, was obviously increased considerably in this study. In comparison, the FDA5,7 requires a minimum of only 1 minute for challenging microbial barriers. The ½ hour challenge time was chosen since at longer challenge the bacteria dries and becomes inactive.
The extreme conditions included the use of a significant number of Equashield® syringes and adapters that were old products with expired use-dates, whereby the sterility of their packaging may have been compromised, as often occurs with old products, and therefore the risk of contamination was much greater than expected from new products that were more recently packaged.
Unlike the conditions in many privileged hospital pharmacies and in previous studies3,4, no cleanroom was used in this study and the laminar flow hood had an open front without the glass screen (which normally improves the isolation of the hood). To maintain equivalence with routine working procedures and conditions in a hospital pharmacy, only one person performed the testing without assistance, and the device packages were opened inside the hood. Furthermore, unlike experienced personnel in hospital pharmacies and previous studies3,4, the operators were not proficient in using Equashield® and only received basic training at the commencement of the study.
The two types of vial accesses, namely: the spiking of the Vial Adaptor onto the vial and the access to the Vial Adaptor with the syringes, were purposely separated in this study. After spiking, the vials were incubated 2 days long and observed for turbidity before syringe accessing began. Both types of vial accesses were effective in preventing microbial ingress.
Furthermore, larger needles are known to cause greater damage and increase leak potential to barrier membranes than thinner needles; therefore Equashield® syringes with the larger needles were used in this study.
Thus, it could be argued that the current study not only reaffirms previous studies results, it also indicates that the solution in the vials remained uncontaminated when using the Equashield® CSTD in even more extreme conditions than may exist in hospital pharmacies, suggesting the possibility of practical benefit from the prevention of the microbial ingress feature, especially for single-use or nonpreserved drugs.
Conclusions
The current study unequivocally demonstrated that Equashield® CSTD is capable of preventing the microbial ingress and contamination of drugs over 7 days of use, which makes it a true CSTD, compliant with both aspects of NIOSH’s definitions2, namely: mechanically prohibiting the transfer of environmental contaminants into the system and the escape of hazardous drug or vapor concentrations outside the system.
Additionally, the standard disinfection procedure using IPA pads on Equashield® access ports was identified as adequate in preventing microbial ingress.
This ability of the CSTD, to provide extended microbial ingress prevention in extreme clinical conditions over a 7 day period, suggests improved patient protection in view of USP Chapter 7971 standards that currently limit the use of single-use non-preserved drugs to up to 6 hours in ISO class 5 air conditions.
Disclaimer
The purpose of this research is to demonstrate the potential use of the Equashield Closed System Device. Its publication does not constitute and must not be construed as promotion or advice to deviate from, alter or otherwise exceed the guidelines, rules and standard related to aseptic preparations and techniques, or in any way deviate, alter or exceed the USE DATE or SHELF LIFE of the drugs. For any modification a user must comply with required steps and measures to change the established guidelines, rules and standard related to aseptic preparations and techniques, such as the procedural changes described in USP 797.
Study reports
- Group 1 test report #680210.1 April 05, 2013; 10 connections and accesses (report attached).
- Group 2 test report #680217.2 April 05, 2013; 7 connections and accesses (on sale).
- Group 3 test report #686405 May 07, 2013; 5 connections and accesses (on sale).
- Group 4 test report #13841-2 April 04, 2014; 5 connections and accesses (on sale).